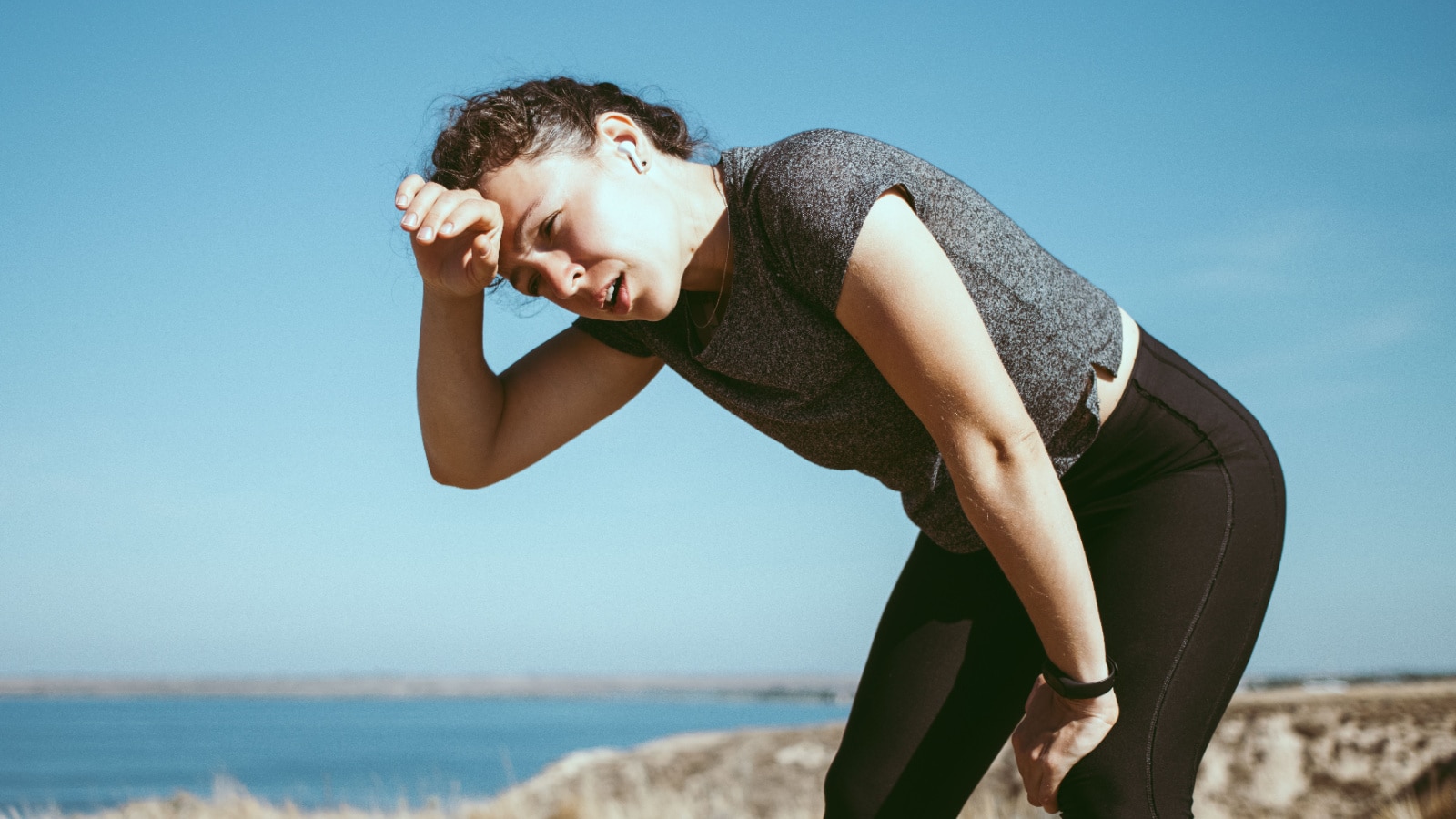
Irritable Bowel Syndrome (IBS) and iron deficiency may occur together and for a few reasons. As we know, IBS causes a symphony of life-altering symptoms including abdominal pain, bloating, diarrhea, and constipation, as well as secondary symptoms like fatigue, anxiety, and low mood. Iron deficiency in its later stages can also lead to tiredness and depressive-type symptoms, which when compounded with IBS is not very much fun!

There may be a few reasons why these conditions occur together including restrictive eating, malabsorption issues, and poor compliance with iron supplements. Let’s explore further about iron deficiency symptoms and risk factors, and how you can help to optimize your iron levels while also managing your IBS so you can feel better, all around!
What is Iron Deficiency and Iron Deficiency Anemia?

It’s important to recognize that iron deficiency is not the same as anemia. The World Health Organization (WHO) defines anemia as a Hb concentration below 12.0 g/dL1. Iron deficiency (ID) is the most common cause of anemia and is defined as the decrease of the total content of iron in the body. Iron deficiency anemia (IDA) occurs when ID is sufficiently severe to reduce erythropoiesis, aka red blood cell production2. However, only one-third to half of iron-deficient individuals have iron deficiency anemia.
Mild-to-moderate iron-deficiency anemia and iron deficiency may present without symptoms. When symptoms do occur, they commonly include:
- Fatigue/ Tiredness
- Weakness,
- Shortness of breath
- Headaches
- Pica: A desire to eat peculiar substances such as dirt or ice
- Hair loss
- Brittle nails
- Cold sensitivity
- Restless Leg Syndrome
- Irritability
- Increased heart rate (Tachycardia)
- Sore or swollen tongue
- Enlarged spleen
Iron deficiency without anemia can also lead to similar symptoms. If you are curious about where your iron stores are at and/or have any of these symptoms, then be sure to speak with your medical doctor to test your ferritin levels. Ferritin is a protein inside your cells that stores iron; the test indirectly measures the amount of iron in your blood which can indicate the level of iron stored in your body.
As a Registered Dietitian, I recommend clients have their iron levels checked at least once a year, and more frequently if they have a history of low iron and/or are at higher risk for low iron. If you have IBS and also experience low energy levels, we recommend having your ferritin levels checked.
Who Is At Risk For Iron Deficiency?

Several factors can contribute to the risk of iron deficiency. Here are some common factors:
- Blood Loss: Any source of significant blood loss can lead to iron deficiency. This may include gastrointestinal bleeding, heavy menstrual bleeding, or injury. People who menstruate and have heavy blood loss are at increased risk for iron deficiency.
- Trouble Absorbing Iron: Malabsorption of iron may be due to gastrointestinal tract abnormalities that are congenital (ie. from birth) or due to surgery. Any changes to the duodenum and/or upper jejunum in the small intestine can impact iron absorption, as this area is iron’s key absorption site.
- Certain Medical Conditions: Medical conditions including inflammatory bowel disease (IBD), celiac disease, and other gastrointestinal disorders, can increase the risk of iron deficiency. Conditions or medications that reduce stomach acid production include using proton pump inhibitors or H. Pylori infection can also decrease iron absorption.
- Poor Nutrient/ Dietary Intake of Iron: Inadequate regular intake of essential micronutrients, including iron, is a risk factor for iron deficiency. This can be particularly relevant for individuals with restrictive eating habits which is often associated with digestive disorders such as IBS.
IBS & Iron Deficiency
Let’s discuss more about the relationship between IBS and iron deficiency. In short, IBS doesn’t cause iron deficiency or iron deficiency anemia, but it does increase your risk.
One of the most common reasons for nutritional deficiencies such as iron in IBS is following a restrictive diet. While we know that the low FODMAP diet can be a lifesaver for IBS, many who follow it do not do so under the guidance of a Registered Dietitian. This can lead to many serious problems including following the Elimination Phase indefinitely (it should only be 2-6 weeks), very limited diet diversity on a low FODMAP diet and/or not properly reintegrating foods back in after the Challenge Phase.
Those who perhaps do not do low FODMAP with IBS may still be following a very restrictive diet due to fears and anxieties around foods they think may cause symptoms, again, without the guidance of a Registered Dietitian which can be very problematic.
A 2022 study looked at the association between symptoms in patients with irritable bowel syndrome, and intake of vitamins and minerals. The study found that intake of micronutrients at baseline was lower than recommended based on national guidelines. Specifically, gastrointestinal symptoms were inversely associated with intake and circulating blood levels of iron. It also found that patient’s blood levels of ferritin were lower in participants who were following a restrictive diet3.
With IBS there is generally no “structural damage” to the intestinal cells that’s associated with celiac or inflammatory bowel disease, however, we now know that some people with IBS may have what is known as “leaky gut” or “intestinal hyperpermeability”. The research is lacking, but one could speculate that this may result in malabsorption issues and also contribute to the risk of low iron or iron deficiency in IBS.
Lastly, we know that IBS can be a debilitating condition that can impact your ability to take care of yourself such as making nutrient-dense meals regularly. In turn, this lack of diet diversity or a nutrient-dense diet can also lead to an increased risk of iron deficiency if your diet lacks iron over a long period.
Can Low Iron Cause Digestive Problems?
Conversely, can low iron or iron deficiency cause digestive problems and symptoms associated with IBS? The short answer is no: there is no research showing that low iron can directly cause gastrointestinal symptoms.
However, iron deficiency may still impact your IBS and digestive health management, as related to our discussion above. Iron deficiency may result in fatigue and low mood, which may impact your ability to care for yourself such as engaging in regular exercise, meal prep, and activities of daily life. So while low iron does not directly cause digestive issues, it may indirectly impact your ability to engage in activities that can help you manage IBS symptoms and have a better quality of life.
How Much Iron Do We Need?

So you may be wondering, how much iron do you need daily? Iron requirements vary based on age, life stage, and gender. Females who are menstruating as well as pregnant or breastfeeding will have higher requirements than males due to increased blood loss and/or blood volume.
Here is a handy reference chart for the Recommended Daily Amounts (RDA) of Iron:

How to Boost Your Iron Levels

So you have been diagnosed with iron deficiency and/or suspect you may have low iron levels and want to boost your iron, how do you do it? Let’s get into the various ways you can support your iron levels so that you can feel better, improve your energy, and avoid those extra symptoms associated with iron deficiency.
Low FODMAP Iron-Rich Foods

Of course, having a nutrient-dense diet regularly is the best way to prevent nutrient deficiencies such as iron deficiency. If you’re following a low FODMAP diet to manage your IBS, there are still ways to ensure your diet is as varied as possible and meet your needs!
Iron exists in food in two different ways: heme iron and non-heme iron. Heme iron is considered highly bioavailable (ie. easy to absorb) and is found in meats and fish. Non-heme iron has low availability and is found in plant-based foods as well as eggs.
Heme Iron Sources:
- Liver (arguably the best source of iron, if you can stomach it!)
- Beef
- Oysters & clams
- Turkey
- Chicken
- Tuna, herring, trout, mackerel
Non-heme Iron Sources:
- Dark leafy vegetables: Swiss chard, spinach
- Seeds: Pumpkin seeds, sunflower seeds, sesame seeds
- Nuts: Macadamia, almonds, pine nuts
- Dark chocolate & cocoa
- Soy proteins: Tofu (firm), tempeh, & edamame (½ cup)
- Legumes: Canned lentils & chickpeas (¼ cup), red kidney beans (2 tbsp)
- Whole grains: Rolled oats, quinoa
- Fortified products (iron added): Low FODMAP bread, cereals or pasta (check the label to see if iron has been added)
- Eggs
We want to focus on a mix of sources when it comes to iron, and we can also increase our absorption of non-heme iron with Vitamin C (more on that below). Those who are following a plant-based diet and do not consume any heme sources are generally recommended to get around 1.8 times above the recommended daily amount of iron to account for the decreased bioavailability of non-heme iron5.
Pair With Vitamin C

As mentioned above, there are two main types of iron found in food. Non-heme iron, found in plant foods, eggs, and dairy products, has a lower absorption rate than heme iron, found in fish and meats. However, we can increase iron absorption by pairing non-heme sources of iron with Vitamin C foods and/or supplements. This is particularly important for vegans and vegetarians who do not consume any sources of heme iron due to avoidance of fish and meats.
Low FODMAP Vitamin C Rich Foods:
- Vegetables: Red bell peppers; green bell peppers
- Berries: Strawberries; raspberries; blueberries
- Citrus: Oranges, kiwi, lemons, limes
- Starchy vegetables: Potatoes (with skin on), sweet potatoes
- Leafy Greens: Spinach, kale, Swiss chard, collard greens, arugula
- Pineapple, cantaloupe & broccoli
Here are some examples of iron and Vitamin C pairing ideas to boost absorption:
- 20g Dark chocolate + 5 strawberries
- 2 kiwis + edamame beans (½ cup)
- Salad with 1 cup baby spinach, ⅓ cup each green and red bell pepper, 2 boiled eggs, ¼ cup canned lentils, and dressing with 1 tbsp each lemon juice and olive oil
Iron Supplements

If you have iron deficiency anemia or low iron levels, you will most likely be recommended to take an iron supplement to help increase your stores in addition to food. Sometimes, food isn’t enough and we may need supplements for a period of time, or intermittently, to ensure iron stores stay within optimal range.
However, if you’ve taken an iron supplement before you probably encountered negative effects on your gastrointestinal system leading you to stop taking it. High-dose iron supplements cause symptoms in the general population, so add IBS onto that and it’s no wonder you may not have stuck with your supplements long-term! The reason for this is that most iron supplements are only absorbed around 25%, and it is the free-floating iron that moves through your gastrointestinal tract that causes symptoms like abdominal pain, constipation and black stools.
The way we can work around this is by choosing the right type of supplement that is gentle and highly absorbable. Liposomal iron is thought to be a superior option, as it is coated in a lipid cell and is absorbed by enterocytes (intestinal cells) rather than in the stomach. As the iron is coated in a lipid cell, it reaches the intestinal tract without losing a lot of nutrients and can be better absorbed there and into your blood. Generally speaking, liposomal iron may have better bioavailability, higher absorption, increased delivery to cells, and consequently decreased gastrointestinal effects6. So this means you’re more likely to actually TAKE your supplement and help increase your iron stores!
I currently recommend Ferosom Forte LCE Liposomal Iron Supplement to my patients who require an iron supplementation to improve their stores, and many of my IBS clients tolerate it very well. Note: their iron supplement sachets contain xylitol which is high FODMAP so I recommend their capsule iron supplements which does not contain any added high FODMAP ingredients. Note that it is a Canadian product.
Use code LEIGH20 at checkout to save 20% off your online order of Ferosom Forte.
I also have had some patients have good success tolerating Ferapro iron supplements, however it is not in liposomal form but may be easier to source in the US.
A word of caution: certain medications and medical conditions such as thalassemia or hemochromatosis may contraindicate taking iron supplements. We always recommend you to speak to your Medical Doctor and Dietitian about iron supplements and the right dose and form for you.
Iron Cookware

Did you know that using cast-iron cookware can increase the level of iron in your food? Yes, that’s right!
Next time you fry an egg, cook a soup or saute vegetables, consider doing so in a cast iron skillet.
You can also use a tool, which is an actual iron “fish”, that can be added to soups, broths, and stews to increase the iron content!
You may want to check out our collection of Low FODMAP Soups Recipes.
Address the Root Causes of Low Iron
Considering the risk factors for iron deficiency and anemia, addressing the cause (s) of low iron losses will also be helpful to ensure you can keep your iron levels within an optimal range. If heavy menstrual cramps are the cause, we recommend speaking to a gynecologist as well as a specialized Dietitian to help address the cause of heavy bleeding.
Further, if unmanaged inflammatory bowel disease or celiac disease is occurring, it would be wise to speak with a gastroenterologist to ensure that these conditions are addressed so that your intestinal tract can heal and best absorb nutrients such as iron moving forward.
If low iron levels are due to a medication, it may be worth considering if that medication is necessary long term or if there are ways that you can better manage the condition and safely come off the medication. For example, Proton Pump Inhibitors (PPI) are commonly used for gastrointestinal reflux disease (GERD) and many patients are left on them long term, without being aware that they increase the risk for low iron and Vitamin B12. For many, there can be simple dietary and lifestyle shifts to manage reflux and symptoms so that the PPI is not required long-term.
Working with a specialized Dietitian can help you to make these changes. It should be noted that we always recommend speaking with your medical doctor before coming off any medications to ensure it is the right decision for you and how to do so safely.
Special Circumstances: Iron Infusions
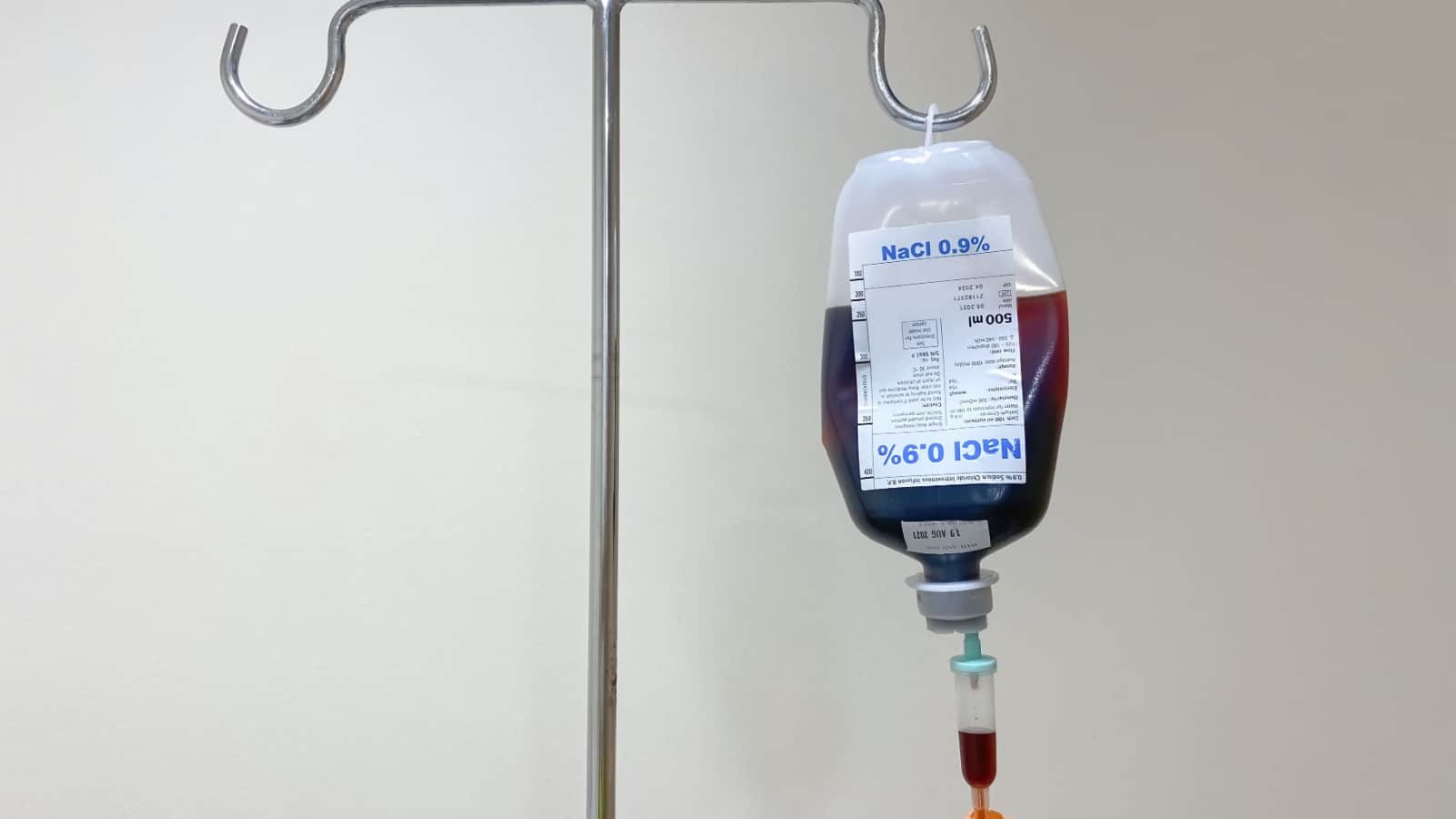
In certain cases, an iron infusion may be necessary to increase iron stores. Taking iron supplements orally (by mouth) is the first preference, as it is less invasive. However, in these circumstances and under the prescription of your medical doctor, an iron infusion may be recommended7:
- Bleeding in the gastrointestinal tract and need to replace iron quickly
- Those with a digestive condition where there is malabsorption of iron and supplements are poorly tolerated such as inflammatory bowel disease (IBD) and celiac disease
- Dialysis patients often lose blood during treatments which results in low iron
- Those who were unable to tolerate oral iron supplements and have low iron
- Anyone who needs to increase their iron level quickly such as in pregnancy or with severe anemia
Depending on where you reside in the world, the state or provincial legal regulations and requirements to receive iron infusions may vary so please speak with your medical doctor if you think this is something that you may require.
Work With a Registered Dietitian

Managing two diseases at the same time can be incredibly overwhelming! Working with a professional can take away some of the pressure and stress while helping you reach your health goals sooner. For help with meal planning, improving iron levels and intake while managing IBS, and improving absorption, consider working with a specialized dietitian. Registered Dietitians are regulated health professionals and are experts in nutrition care and medical nutrition therapy. Visit our Global Dietitian Directory to find the right fit for you.
Conclusion

As you can see, there is an interesting intersection between IBS, iron deficiency, and anemia. While it may seem complicated to manage these conditions together, fortunately, there are many overlapping strategies to help both your IBS symptoms as well as improve your iron levels.
As we’ve mentioned, if you want to manage both your IBS and iron deficiency/anemia and adequate nutrient levels, consider working with a Registered Dietitian on your health journey!
Summary:
- Irritable Bowel Syndrome (IBS) and iron deficiency can coexist, potentially due to factors such as restrictive eating habits, malabsorption issues, reduced energy for self-care activities, and poor compliance with iron supplements.
- Iron deficiency is not the same as anemia, and only a portion of iron-deficient individuals develop iron deficiency anemia (IDA).
- Symptoms may not be present in mild-moderate iron deficiency and iron deficiency anemia. If they are present, common symptoms of iron deficiency and IDA include fatigue, weakness, shortness of breath, headaches, pica, hair loss, and more.
- IBS doesn’t directly cause iron deficiency or IDA but increases the risk, particularly when following restrictive diets or experiencing malabsorption issues.
- Strategies to manage both IBS and iron deficiency include consuming iron-rich foods, pairing iron sources with vitamin C for better absorption, considering gentle and absorbable iron supplements like liposomal iron, using iron cookware, addressing root causes of low iron, and, in severe cases, considering iron infusions under medical supervision. Working with a Registered Dietitian is recommended for comprehensive management of these conditions.
References
- Mansour, D., Hofmann, A., & Gemzell-Danielsson, K. (2021). A review of clinical guidelines on the management of iron deficiency and iron-deficiency anemia in women with heavy menstrual bleeding. Advances in therapy, 38, 201-225. ↩︎
- Bermejo, F., & García-López, S. (2009). A guide to diagnosis of iron deficiency and iron deficiency anemia in digestive diseases. World journal of gastroenterology: WJG, 15(37), 4638. ↩︎
- Roth, B., Larsson, E., & Ohlsson, B. (2022). Poor intake of vitamins and minerals is associated with symptoms among patients with irritable bowel syndrome. Journal of Gastroenterology and Hepatology, 37(7), 1253-1262. ↩︎
- Iron-deficiency anemia. (2022, March 24). National Heart Lung and Blood Institute. ↩︎
- Pawlak, R., Berger, J., & Hines, I. (2018). Iron status of vegetarian adults: a review of literature. American journal of lifestyle medicine, 12(6), 486-498. ↩︎
- What does liposomal mean and how can it help my iron deficiency?. (2021, August 9). Ferosom Forte. ↩︎
- Iron infusion. (2023, August 30). Cleveland Clinic. ↩︎







Cast iron cookware helps? That is very interesting and since so many people have opted for lighter weight cookware due to convenience I can understand why there may be more suffering from Low iron now than in the past.
Very interesting article ,glad to have read it!
Hi there Linda. I know some people, as they get older, find cast iron to be heavy. On the other hand, I know people who are very much interested in cooking (me included) and would not give up their cast-iron or enamel cast iron. Glad you found helpful info!