The Truth Is In the Timing: What Your Digestive Reaction Time Can Reveal About the Cause of Your Adverse Food Reaction
I’ve been a dietitian working in a gastroenterology practice for almost a decade, where I spend my days listening to the gory details of meals gone awry. Through this experience, I’ve come to realize that many people who suffer from a chronic digestive problem are pretty good at identifying which food(s) seem to trigger their symptoms.
But what they’re less likely to get right is the reason why these foods provoke their symptoms – and how the timing of digestive symptoms can be part of diagnosing the root cause.
- The Truth Is In the Timing: What Your Digestive Reaction Time Can Reveal About the Cause of Your Adverse Food Reaction
- What's To Blame? Seeking Answers.
- REACTION TIMING
- Reaction Time: Zero to Fifteen Minutes
- Reaction Time: Fifteen to Ninety Minutes
- Signs of Potential SIBO
- Reaction Time: Two to Eight Hours
- When The Low FODMAP Diet Can Make Symptoms Worse
- Diagnose The Actual Root Cause
- And The Clock Keeps Ticking
- Read All Of Tamara's Articles:
What’s To Blame? Seeking Answers.
It’s The Dairy! Or Is It?

“Dairy” is a common scapegoat when, say, ice cream provokes diarrhea within minutes of consuming it – but these same patients will also acknowledge that not all dairy foods seem to have this effect.
I Know It’s The Gluten/Corn Allergy/Bacteria/Food Poisoning!

“Gluten” also gets the blame for a lot of digestive system reactions, though patients will admit that some forms of gluten don’t seem to trigger symptoms as much as others…and usually, they still suffer symptoms even when they completely avoid it.
I’ve had patients who see corn in their loose stools assume they’re “allergic” to corn, and I’ve seen patients who experience immediate indigestion upon eating something blame it on bacteria in their intestines.
Some patients prone towards diarrhea and cramping after restaurant meals assume that they just keep getting food poisoning again and again—even though no one else at the table ever gets sick, too.
In this context, my job is often to help people connect the dots between effect and cause so they can eliminate the foods that actually disagree with them, while preventing excessive restriction of foods that don’t.
To do this detective work, I probe for details about the timing of a person’s symptoms relative eating certain foods. As you will see, this relationship offers important clues as to the most likely causes of a symptom – and most importantly for our purposes, provides actionable insights into how to manage those symptoms through diet change.
You May Want To Read: The Low FODMAP Diet Is Not A Gluten-Free Diet
REACTION TIMING
Reaction Time: Zero to Fifteen Minutes
A near instantaneous adverse reaction to food typically signals an immune system or biochemical reaction to a component in that food rather than a food intolerance happening in the intestines.
After all, in this brief time period, your meal has not yet had the chance to empty the stomach and begin its intestinal journey. Therefore, such rapid adverse food reactions cannot be generally be blamed on malabsorption or bacterial fermentation as would be the case from, say lactose intolerance or another FODMAP intolerance.
Such a rapid response to food can be mobilized by the immune system in response to foreign proteins it recognizes as allergens, however. If you have a classic food allergy, in which you have elevated levels of IgE antibodies to a food protein, you could react within minutes of ingesting the trigger food – and that reaction could manifest in gastrointestinal symptoms like acute stomach pain, vomiting or diarrhea.
You May Want to Read: Food Allergy vs. Food Intolerance: Navigating a Complicated Path
We often think of food allergy as a phenomenon of childhood – and one that many kids outgrow to some extent. But adult-onset food allergy seems to be on the rise, and a recent population-based survey published in JAMA Network Open found that close to 11% of American adults have a food allergy.
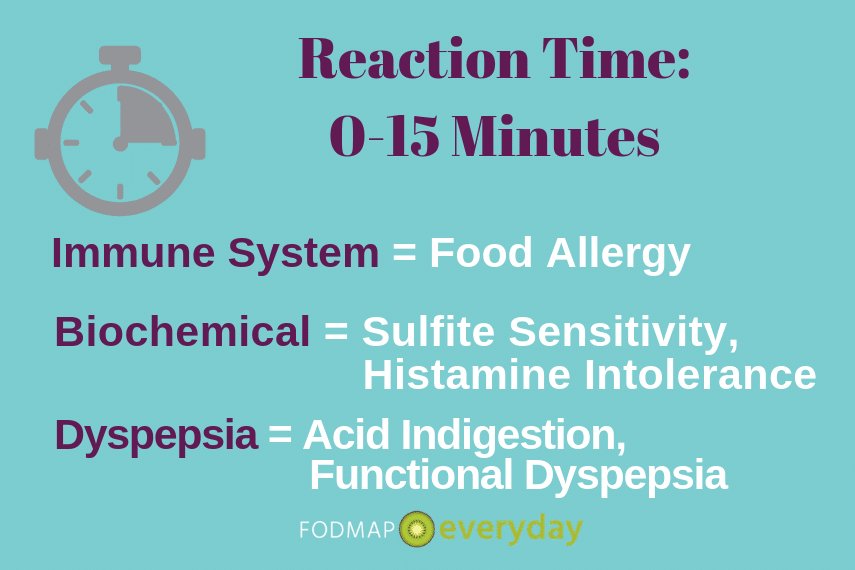
Another possible cause of quick-onset digestive system reactions to food can be biochemical reactions to components in the food. Examples of this can include:
Sulfite Sensitivity
- Sulfite Sensitivity, in which affected people can experience anything from asthma attacks and hives to sudden onset abdominal cramping and diarrhea when consuming foods or alcoholic drinks preserved with foods additives called sulfites.Avoiding foods that contain sulfites – like dried fruit, red wine and a variety of condiments and frozen foods – is the remedy for this reaction.
Histamine Intolerance
- Histamine Intolerance, in which affected people can experience symptoms throughout the body within minutes of consuming a food that contains high levels of a nitrogen-containing compound called histamine. When consuming high histamine foods – from tomatoes and spinach to aged cheeses and other fermented foods – some of my affected patients may start to experience almost immediate onset abdominal bloating (distension), stomach pain, feelings their throat or chest tightening, and/or heart palpitations. (Other histamine related symptoms may take slightly longer to kick in, but among them are headaches, lightheadedness, fatigue, flushing, hives or itchiness, and/or diarrhea.)
A low histamine diet can help control such food reactions, often with support from a histamine blocking regimen taken under the supervision of a well-credentialed allergist/immunologist or gastroenterologist.
Dyspepsia
Finally, various types of Dyspepsia can lead to rapid onset upper digestive distress after eating, including upper abdominal gas (belching), excessive fullness, heartburn, nausea and even upper stomach pain.
- People prone to Acid Indigestion can experience these symptoms due to acid reflux, which may be triggered by eating larger meals, higher fat meals or foods known to reduce the pressure of the muscle that separates the stomach and the esophagus. These include alcohol, mint, onions, garlic, coffee and chocolate.
- People with Functional Dyspepsia can experience similar symptoms even in the absence of acid reflux. Rather, their discomfort results from the stomach’s impaired ability to stretch adequately in response to eating – possibly worsened by hypersensitive nerve signals in the digestive tract. Eating small, soft textured meals more frequently can help manage symptoms of this condition, and certain over-the counter remedies like FDGard or Iberogast have been shown to be helpful as well.
Reaction Time: Fifteen to Ninety Minutes
While the allergic or biochemical reactions described above can still take place in this 15 to 90-minute window of time, by now food has started emptying into the small intestine.
This opens up other possibilities in terms of the cause of your adverse food reactions.
Accelerated Gastrocolic Reflex (GCR)
People with Irritable Bowel Syndrome (IBS) who find themselves running to the bathroom with crampy diarrhea very soon after eating larger meals, higher fat meals or bulky, high volume foods like salads or popcorn are often experiencing the effects of an accelerated gastrocolic reflex (GCR).
The GCR is a normal digestive system nerve signal between the upstream portion of your digestive tract and the downstream portion of your digestive tract.
In response to greater stretch of the stomach and/or the arrival of fat into the small intestine, a message is sent to the colon that warns it of the meal coming down the pipeline that may need to be accommodated. (This is why we often poop soon after meals rather than spontaneously at random times of the day.)
Larger stretch or more fat can send a stronger signal and therefore a stronger urge to defecate – and for people with IBS, whose digestive system ‘thermostat’ is already extra-sensitive, the gastrocolic reflex can send a pretty forceful message to the colon at even lower thresholds of upstream stimulus.
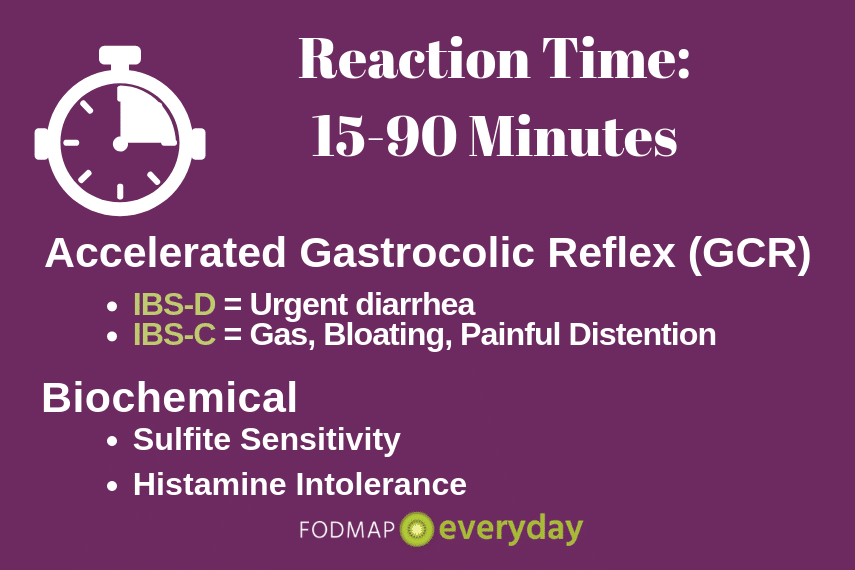
For people with diarrhea-prone IBS, this may result in urgent, crampy diarrhea very soon after eating, and the notion that “salads run right through me,” though it’s not actually the salad you just ate that you’re pooping out.
For people with constipation, this may result in gas pain, visible distension of the belly and/or excess farting as the intestinal pipeline fills up with more substance and the stool in the colon is moved along…but the body is unable to actually pass a bowel movement and free up space.
People with milder cases of IBS often find that simply watching meal portions, avoiding (or limiting portions of) ‘roughage,’ and avoiding higher fat meals can keep this symptom in check. When diet modification fails, well-timed antispasmodic supplements (such as enteric coated peppermint oil) or prescription medications can be hugely helpful.
Signs of Potential SIBO
People who experience mid-to-lower abdominal gas pain, excess farting, rumbling gas noises and/or bloating that may or may not be accompanied by an urgent bowel movement in this time frame could also be looking at a case of Small Intestinal Bacterial Overgrowth (SIBO).
This is particularly the case if the foods that provoke such symptoms are high in either fat or FODMAPs. One way to differentiate between an accelerated GCR as described above and SIBO is how you react to bulky/fibrous but low-FODMAP foods like popcorn or a basic garden salad: people with classic IBS are more likely to find that these foods provoke their symptoms, whereas those with SIBO may actually find these foods to be relatively well tolerated.
You May Want To Read: SIBO: Get the Facts
Reaction Time: Two to Eight Hours
The onset of intestinal gas (especially foul-smelling gas), gas pain, bloating and/or loose stools—especially lighter colored, malodorous or ‘acidic feeling’ stools – in the 2-to-8 hour window following a meal is more like to be malabsorptive in nature.
This is because the meal is starting to move out of the small intestine – where any nutrients that can be absorbed have been absorbed – and the remaining waste is now entering the colon and encountering a huge community of bacteria.
Two hours is on the earlier side of the typical reaction time and is more likely to occur if you’ve consumed the offending food on an empty stomach or in liquid form; a more typical reaction time for food consumed in a mixed, solid meal is 4 to 8 hours.
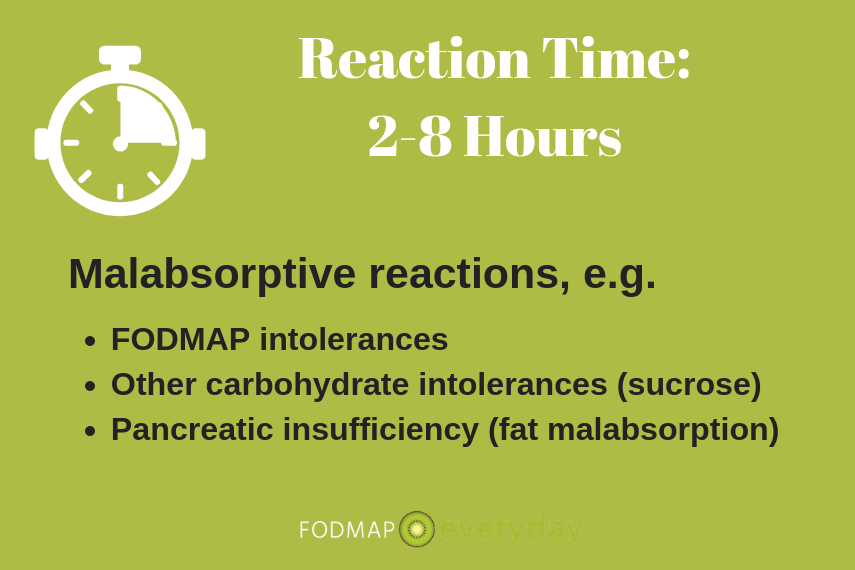
Gas, Gas, & More Gas
The more available nutrients that remain in the waste stream – whether undigested sugars like lactose, fructose and sorbitol or undigested fibers like the fructans in onions and garlic or the oligosaccharides in beans and brussels sprouts – the more gas your gut microbiota can generate.
This gas can last for hours as the undigested material makes its way through the colon, and its severity will vary based on how much of that food you consumed. In the biz, we refer to these reactions as carbohydrate intolerances, of which “FODMAP intolerance” is counted among them.
When The Low FODMAP Diet Can Make Symptoms Worse
A rarer – and therefore less commonly recognized – form of carbohydrate intolerance is sucrose isomaltase deficiency (SID); it is an enzyme deficiency that produces digestive symptoms in response to foods that contain sucrose (table sugar) or simple starches like rice, bread, oats, potatoes, bananas and sweet potatoes. Because many of these foods are staples on the low FODMAP diet, people who find themselves experiencing worsening of symptoms after trying out the low FODMAP diet might consider exploring their food/symptom reactions with an experienced GI dietitian and pursuing testing for SID.
Diagnose The Actual Root Cause
In all of these cases, pinpointing the exact nature of the intolerance through breath testing (when available) and/or a FODMAP elimination diet followed by a controlled re-challenge protocol will help steer you toward a precise list of foods to avoid and limit unnecessary dietary restriction.
In some cases, over-the-counter digestive enzymes may be available to help improve absorption of the trigger carbs and eliminate the need to avoid them entirely. For example, lactase enzyme can minimize symptoms associated with lactose intolerance; xylose isomerase can minimize symptoms associated with fructose intolerance, and alpha galactosidase can help with symptoms associated with foods rich in the GOS family of FODMAPs.
While carbohydrate intolerances are the most common form of malabsorption – and malabsorptive symptoms – other types of malabsorption can provoke similar GI symptoms in this time window as well. People who do not produce enough pancreatic digestive enzymes—a condition known as pancreatic insufficiency—can experience malodorous gas, gas pain, diarrhea and often weight loss as well—in the 2-8 hours after consuming anything—but fats in particular. A simple stool test can diagnose pancreatic insufficiency, and prescription enzymes should remedy the situation.
And The Clock Keeps Ticking
It’s dicey to attribute a particular digestive symptom to a food you consumed more than 8 to10 hours prior, as by that time, you’ve presumably consumed at least one if not several other meals and snacks whose contribution to your symptoms cannot be ignored.
While it’s not uncommon for someone to have symptoms in the morning related to something they had for dinner the previous evening, it would be very difficult to find a mechanism by which something you ate a day ago (let alone two or even three) would start wreaking havoc on your digestive tract more than a half a day later.
To be clear: since it can take a full 72 hours total transit time from the time you eat something for its residual waste to be eliminated, it’s possible that a symptom like excess gas and bloating could start within the 10 hour window and last for a few days. But if a symptom suddenly appears, you shouldn’t be looking to what you ate three days ago to account for it.
Because it can take up to 72 hours for a food that has triggered a digestive reaction to completely clear the body, people who are testing tolerance for high FODMAP foods after an initial elimination phase are generally advised to take a three-day break after failing a FODMAP challenge before testing something new. This spacing will help ensure that you don’t confuse the cause of symptoms you experience between a previously-tested food and a new-to-test food.
Please also check out Tamara’s other articles on Gut Microbiome Testing, Are You Full of Sh*t, and also on Bloating.
And if you are struggling with determining the cause of your bloating and how to manage it once and for all, then be sure to grab Tamara’s best-selling book: The Bloated Belly Whisperer available through Amazon US, UK, CA and AU.
Read All Of Tamara’s Articles:
- What Conventional Wisdom Gets Wrong About Bloating
- Timing of Digestive Symptoms: What It Means
- What Is Leaky Gut Syndrome?
- Are You Full of Sh*t? Stool Burden and the Low FODMAP Diet
- Everything You Want to Know About Farting*
- 5 Reasons to Skip Gut Microbiome Testing – For Now
- Exclusive Interview with Dietitian Tamara Duker Freuman
- Q & A With The Author Of “Regular, The Ultimate Guide to Taming Unruly Bowels and Achieving Inner Peace”
Looking for a dietitian?
We always recommend working with a low FODMAP experienced Registered Dietitian. You can check out our directory to find one near you. Many of them will work online and remotely with you so be sure to reach out to anyone within your area.






I really enjoyed this article it has given me a lot to consider resolving some personal digestive distress.
My husband has Celiac disease and it took us about 6 yrs and several different doctors to figure it out. The biggest factor being the delayed response time from when he ate the trigger food gluten. His reactions come 24-48 hrs after. It seems like the delayed reaction of a celiac response should be mentioned in an article on digestive timing.
Thank you for the suggestion. The article is focused on FODMAPs, but we will take this into consideration and discuss with our dietitians.
I was super excited to find this after researching for so long, however still can’t find an answer out there. Haha. I eat very consciously and have come a long way with a lot of digestive disorders after being on antibiotics for a week in the hospital a few years back. At this point, my histamine response happens almost 8 hours on the dot after eating. If I eat in the morning, and wait, 8 hours later, hives and extreme panic attacks will kick in. If I eat at 6 at night, it will happen around 2am. I actually called the ambulance once which is WAY not something I would usually do, but it was a bad reaction and I wasn’t sure if it was a heart attack in that moment. If I don’t eat high histamine foods, I am fine and will not experience them at all. If I eat something high in histamine though, it happens every time even though I take dao. Any thoughts?
Thanks so much!!
Hi there, we do not give medical advice but we can tell you that is exactly the kind of situation that a dietitian can help with. Please do consider working with one. You do not even have to have one near you, as so many to telehealth appts. these days.
I have been diagnosed with IBS and the low fodmap diet works very well for me. I’ve found I can tolerate a few things on the list. Recently I found Fodzyme, an enzyme mix, which has changed my life because I can now eat out and travel, just by sprinkling a bit of the powder on the meal before eating. It has worked on everything I’ve tried it on so far. I bought it on line but am not sure if it’s available at chemists.
Hi Frances, we love FODZYME! We just completed a Webinar with them. Check it out here.
I often get discomfort low down on left tummy which starts approx 3 or 4 hours after dinner. I eat at 6pm. That will often pass after an hour or two, then come back later sometimes. No symptoms higher up and no bloating. Passing wind helps. The wind has NO smell at all! This never happens after my small plain breakfast/brunch at 11am (just toast butter and honey) but always after eating vegetables at 6pm. Morning bowel movement often a bit loose but again no bad smell and normal colour etc. The more veg I eat the looser my bm. Fats don’t seem to bother me, or simple carbs. I wondered what this is. It doesn’t happen all the time, just sometimes, and I eat from the same range of foods all of the time, nothing unusual.
Hi there, we do not give medical advice, but the diet is meant to be overseen by a Registered Dietitian, and this is exactly the type of thing they can trouble shoot with you.
I noticed my colleague and I are not in your Monash FODMAP trained dietitian list. Wondering how we can be added to that?
Hi there, check THIS PAGE and there is a button that says Fill Out This Form.