Hype vs. Fact
There has been a lot of hype in the gut health world over the past few years about the benefits of probiotics for any number of GI issues, including IBS (irritable bowel syndrome).
But, what’s the bottom line? Should you take a probiotic supplement alongside other treatments for IBS, such as the low FODMAP diet? And if so, which one and when? This article will explore the latest science in attempting to answer these questions.
What Are Probiotics?
According to International Scientific Association for Probiotics and Prebiotics (ISAPP), a probiotic is defined as “live microorganisms that, when administered in adequate amounts, confer a health benefit on the host[1]” or, in layman’s terms, bacteria or yeasts that can offer health benefits (such as improving digestive or immune health) when consumed in sufficient amounts.
They Must Be Live
Some people also talk about probiotics as being “good bacteria” versus pathogenic or infection-causing bacteria. An important key word in the definition is “live,” because to provide any benefit, the bacteria must survive the journey through the GI tract into your colon.
Our stomachs tend to be very acidic and not all bacteria will survive long enough to deliver any specific benefits to us. The quantity of bacteria is important too, as just a few doesn’t count as a probiotic and really won’t really do the job.
How Do Probiotics Work & What Can You Expect?
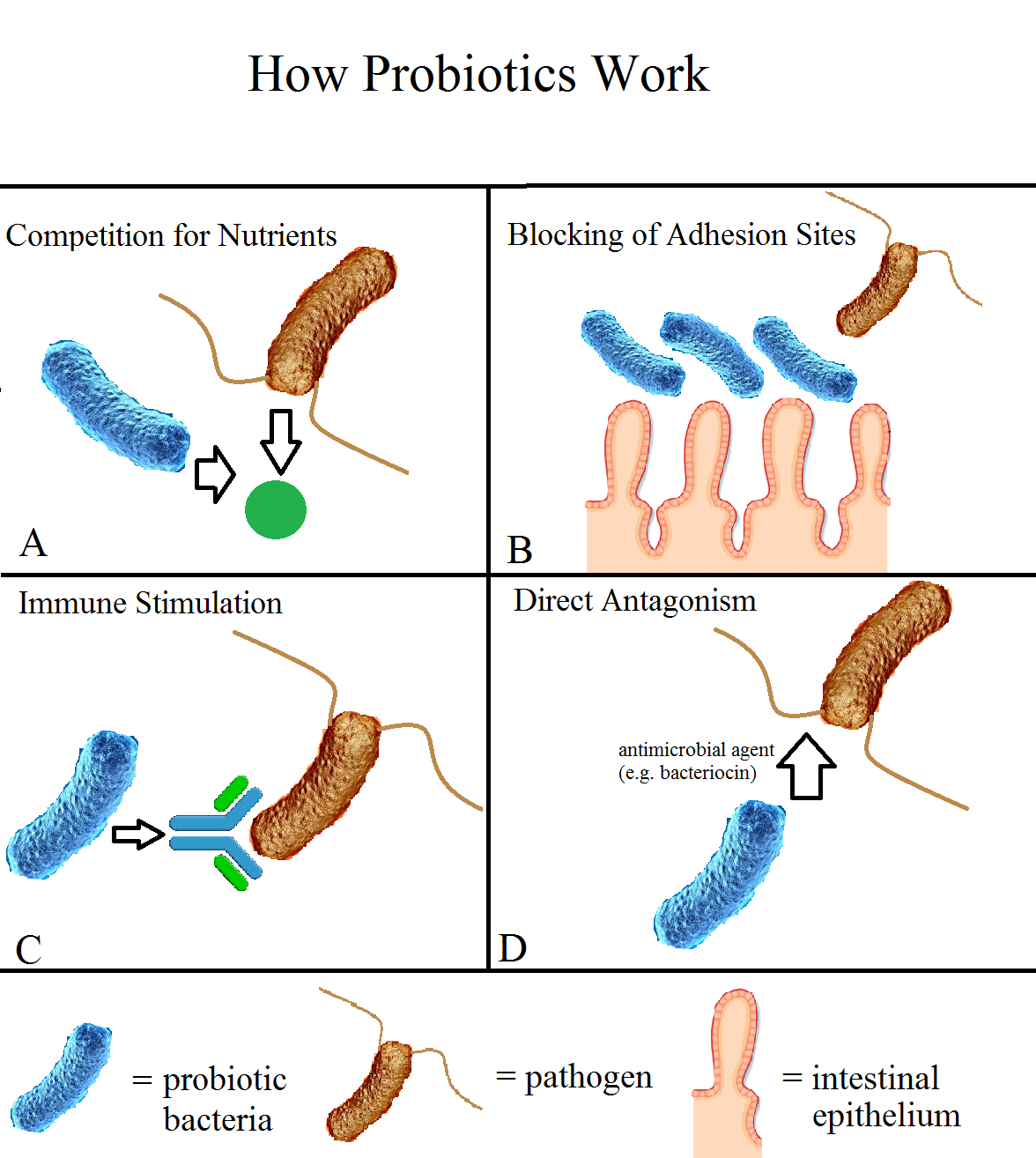
There are a number of ways that probiotics interact with our gut. For example, taking a specific probiotic blend may help populate the gut with helpful bacteria that may be missing or in short supply in certain individuals.
It is well known that individuals following a low FODMAP diet may have reduced numbers of Bifidobacteria due to decreased intake of prebiotic fiber, so a probiotic supplement containing this species can help maintain levels in the gut[2].
In addition, probiotics can increase production of short-chain fatty acids in the colon, which can decrease intestinal pH and enhance the barrier function of the epithelium (these are the cells that line the stomach and intestines)[3].
Certain strains of bacteria may also help increase the production of B-galactosidase which can help individuals better digest lactose[4], while other bacterial strains may serve to reduce markers of inflammation in the gut or provide an anti-depressant function by increasing levels of serotonin.[5]
Finally, certain probiotic bacteria that can reduce colonic transit time or improve visceral hypersensitivity[6].
Improvements in IBS Symptoms
These effects on the gut can translate to improvements in IBS symptoms, such as reduced gas and bloating, improved stool consistency, decreased abdominal pain, improved diarrhea or constipation, overall symptom relief and/or enhanced quality of life.
It’s important to note that different types of bacteria may affect the gut in different ways, such as Bifidobacterium and Lactobacillus, which are two of the most studied probiotic bacterial species for gut health.
It’s also possible that probiotics may be more effective in individuals who have evidence of microbiome alterations, such as in the case of post-infectious IBS (e.g. onset of IBS following a bout of food poisoning or gastroenteritis[7]).
Which Probiotic to Take?
In the highly variable world of IBS symptoms, what helps one person may have no effect for another. While researchers are very focused on this aspect of gut health, what we don’t know is still far more than what we do know.
[bctt tweet=”The effectiveness of a probiotic will depend on your own unique gut microbiota, your age, diet and exercise levels, genetics, stress levels and your specific IBS symptoms.” username=”FODMAPeveryday”]
What to Consider When Purchasing a Probiotic Supplement:
- Brands: The brands often recommended by GI dietitians in the US include Align, Culturelle (look for a version like this one without chicory root, which is high in FODMAPs), Good Belly, Symprove and VSL #3, as there is scientific research that supports the use of these for IBS. Some probiotics may work better for IBS-D versus IBS-C, so you may need to experiment a little to find one that works for you.
- Format: Probiotics come in many formats, including beads, capsules and powders. Use the form that works best for you. Be sure to purchase a freeze-dried or enterically-coated probiotic supplement to ensure the bacteria make it through your GI tract alive and in sufficient numbers. Also, check the label for the expiration date as probiotics may not be useful past this date.
- Dose: Probiotic supplements typically are labeled with the number of colony forming units (CFUs) contained in each serving. CFUs are the number of bacteria (or yeast) that are capable of living and reproducing to form a new group of the same bacteria or yeasts[8]. As discussed above, the number of bacteria is important, because without sufficient numbers of live bacteria, the product is not likely to have any effect. A general rule of thumb, based on previous studies[9], [10], is a minimum of at least 100 million to 1 billion CFUs per daily dose[11], though there is currently no known “optimal” dose.
- Single or Multiple Strain: Supplements that contain a blend of several bacterial strains (such as VSL #3) may be more effective than a single bacterial strain, however this does depend on your symptoms[12]. In some cases, a single strain may work best.
- Watch Out! Some probiotics also contain prebiotic (a substrate that is selectively utilized by host microorganisms conferring a health benefit[13]) fiber, such as inulin, chicory root, GOS or FOS (galacto- or fructo-oligosaccharides), which are high in FODMAP, so be sure to read labels carefully!
- Where to Buy: You can purchase probiotic supplements in most pharmacies or chemists, as well as in health food or natural foods stores and via online pharmacies or major sites like Amazon (which has a FODMAP Everyday® store front for your low FODMAP diet needs). Or in our shop where we have curated all of the low FODMAP nutritional supplements in one easy to navigate shop. Look for a quality brand name and ideally, one that has been tested for potency.

We have curated all of the low FODMAP nutritional supplements in one easy to navigate shop.
When Should You Consider a Probiotic?
Monash University recommends individuals following the low FODMAP diet wait until after the Elimination and Challenge phases are complete before introducing probiotics, as they can “muddy the waters” when it comes to figuring out which specific foods are triggering IBS symptoms.
Introducing probiotics or other supplements during Elimination can exacerbate symptoms or cause issues that weren’t present before.
If your doctor or dietitian has recommended a probiotic and asked you to continue it during the Elimination phase, you may wish to discuss with them the pros and cons of taking a probiotic during Elimination, to identify together what’s best for your individual situation.
How to Take Probiotics
While probiotics are generally considered safe for daily use, it’s important to read product labels for the appropriate daily dose and follow your healthcare provider’s recommendation. Remember that more isn’t always better and can actually trigger symptoms rather than relieve them.
It is recommended to take probiotics with a meal, as the food you eat also provides the bacteria with the food they need to thrive and reproduce. In addition, having some food can provide a bit of a buffer against stomach acid, helping increase the chances of survival of the live bacteria as it passes through your GI tract[14].
Finally, trial probiotics for a minimum of 4 weeks, as it can take some time to see benefits.
[Note: Probiotics are not recommended for children or immune-compromised adults without first consulting a healthcare provider, as there can be adverse side effects or dosage concerns.]

The Bottom Line
Probiotics are not a magical cure-all for IBS, but they can be yet another tool in your toolbox (alongside other treatments and modalities such as the low FODMAP diet, exercise and meditation) to help you live a happier, more active and pain-free life!
Final Note: Please speak with your doctor or dietitian before taking a supplement to discuss whether probiotics might make sense for your specific symptoms and which one might be best for you. Feel free to use this article as a “jumping off point” for your discussion!
For more helpful articles authored by Diana Reid, RDN to help you with your FODMAP journey, check out Getting Started on The Low FODMAP Diet as well as an article to help you navigate Exercise, while dealing with IBS.
References
[1] Hill, C. et al. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nature Reviews Gastroenterology & Hepatology 11, 506–514 (2014).
[2] Staudacher, H. M. et al. A Diet Low in FODMAPs Reduces Symptoms in Patients with Irritable Bowel Syndrome and A Probiotic Restores Bifidobacterium Species: A Randomized Controlled Trial. Gastroenterology 153, 936–947 (2017).
[3] Aragon G, Graham DB, Borum M, Doman DB. Probiotic Therapy for Irritable Bowel Syndrome. Gastroenterology & Hepatology. 2010;6(1):39-44.
[4] Hill, C. et al. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nature Reviews Gastroenterology & Hepatology 11, 506–514 (2014).
[5] Aragon G, Graham DB, Borum M, Doman DB. Probiotic Therapy for Irritable Bowel Syndrome. Gastroenterology & Hepatology. 2010;6(1):39-44.
[6] Verna, E. C. & Lucak, S. Use of probiotics in gastrointestinal disorders: what to recommend? Therapeutic Advances in Gastroenterology 3, 307–319 (2010).
[7] D., C. et al.Postinfectious Irritable Bowel Syndrome | Clinical Infectious Diseases | Oxford Academic. OUP Academic (2008). Available at: https://academic.oup.com/cid/article/46/4/594/298845. (Accessed: 27th April 2018).
[8] CFU: What Does Colony Forming Unit Mean? Does It Matter in Probiotics? PowerOfProbiotics.com. Available at: https://www.powerofprobiotics.com/Cfu.html. (Accessed: 27th April 2018).
[9] Katzka, D. Efficacy of an Encapsulated Probiotic Bifidobacterium infantis 35624 in Women with Irritable Bowel Syndrome. Yearbook of Gastroenterology2007,36–37 (2007).
[10] Verna, E. C. & Lucak, S. Use of probiotics in gastrointestinal disorders: what to recommend? Therapeutic Advances in Gastroenterology 3, 307–319 (2010).
[11] Probiotics | Science-Based Probiotic and Prebiotic Information | ISAPP. International Scientific Association for Probiotics and Prebiotics (ISAPP)Available at: https://isappscience.org/probiotics/. (Accessed: 27th April 2018)
[12] Hungin, A. P. S. et al.Systematic review: probiotics in the management of lower gastrointestinal symptoms – an updated evidence-based international consensus. Alimentary Pharmacology & Therapeutics47,1054–1070 (2018).
[13] Gibson, G. R. et al. Expert consensus document: The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nature Reviews Gastroenterology & Hepatology (2017). doi:10.1038/nrgastro.2017.75
[14] Greger, M. How Should I Take Probiotics? NutritionFacts.orgAvailable at: https://nutritionfacts.org/2014/01/02/how-should-i-take-probiotics/. (Accessed: 27th April 2018)




June 9, 2020
American Gastroenterological Association (AGA) does not recommend the use of probiotics for most digestive conditions
“There was insufficient evidence for AGA to make recommendations regarding the use of probiotics to treat C. difficile infection, Crohn’s disease, ulcerative colitis or 𝐈𝐁𝐒. For these conditions, 𝐀𝐆𝐀 𝐬𝐮𝐠𝐠𝐞𝐬𝐭𝐬 𝐭𝐡𝐚𝐭 𝐩𝐚𝐭𝐢𝐞𝐧𝐭𝐬 𝐜𝐨𝐧𝐬𝐢𝐝𝐞𝐫 𝐬𝐭𝐨𝐩𝐩𝐢𝐧𝐠 𝐩𝐫𝐨𝐛𝐢𝐨𝐭𝐢𝐜𝐬, as there are associated costs and not enough evidence to suggest lack of harm.”
https://gastro.org/news/aga-does-not-recommend-the-use-of-probiotics-for-most-digestive-conditions-2/
As a science based individual it is strange you don’t allow a more recent review of the probiotic RCT’s by the AGC released in June 2020 – it more recent that any of the studies referenced on this web page. The details of the complete technical review are provided in this article. The one I posted earlier was an overview
See the answer to the question “Question 6: In Symptomatic Children and Adults With Irritable Bowel Syndrome, Should Probiotics Be Used to Improve Global Response or Abdominal Pain Severity?”
“Given the numerous individual probiotic strains that demonstrated benefit in the context of a single trial, one cannot exclude a potential benefit of probiotics for children and adults with IBS. However, the Technical Review Panel also identified numerous registered protocols that had neither peer-reviewed publications nor raw data available for review, highlighting the potential for publication bias. Although the breadth of data regarding probiotic use for IBS is substantial, no single strain or combination has been studied in a sufficiently rigorous manner.”
https://www.gastrojournal.org/article/S0016-5085(20)34732-6/fulltext
Certain strains of probiotics have been shown useful in certain cases. As always, it’s best to discuss your specific situation with your healthcare team in order to identify the treatment strategy that works best for you.
And Monash follows up with a similar comment “What recommendations can be made about the use of probiotics for IBS? A guideline published by the American Gastroenterological Association in 2020 concluded that there is currently insufficient high-quality evidence to make recommendations about the use of probiotics to treat IBS. ”
https://www.monashfodmap.com/blog/probiotics-ibs-update/
Please see our other response, which is also based upon clinical experience by Monash and King’s College trained dietitians.